
Isaac Lauper in physical therapy following his spine surgery.
At the tender age of 24 hours old, Isaac Lauper underwent his very first surgery at Akron Children’s. Born with spina bifida myelomeningocele (a neural tube defect where the spine is exposed), Isaacs’s spine needed to be surgically closed after birth. Due to many other conditions that are secondary to his spina bifida, Isaac has had dozens of surgeries and procedures over the years since then.
At age 8, Isaac had developed a severe kyphosis (a form of scoliosis) or kinking of his back – a deformity common to patients with myelomeningocele. He was referred to orthopedic surgeon Dr. Todd Ritzman.
According to Isaac’s mom, Julie, “The hump in his back was very prominent. It would rub on things and cause his skin to open. Isaac wasn’t able to sit up straight, and this caused a lot of problems with his digestion and swallowing. He was throwing up daily.”
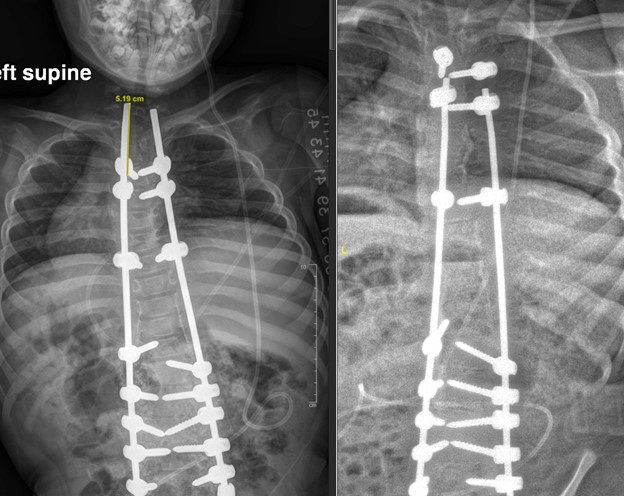
(Left) X-ray of Isaac’s spine immediately after surgery at age 8. (Right) X-Ray of Isaac’s spine at age 13. The spine has successfully grown off of the rods as guided by the Shilla implants. Isaac’s spine remains well aligned and he should not require additional surgery.
Dr. Ritzman says Isaac needed surgery to correct the deformity, but he was too young for a definitive spinal fusion procedure because he needed more growth of his thorax and lungs. Instead, he recommended a complex resection of Isaac’s kyphotic vertebrae, with limited fusion of his lower spine. This growth-friendly procedure ensured satisfactory alignment while he completed his growth.
“The Shilla procedure enables control of a spinal deformity through fusion of the primary location of the deformed spine while permitting continued growth of the remainder of the spine,” said Dr. Ritzman. “This enables relatively small spinal fusions to be performed through smaller open procedures while guidance of spine alignment during growth is enabled through implants placed percutaneously throughout the remainder of the spine.”
Patients with congenital or neuromuscular scoliosis (myelomengocele, cerebral palsy, etc.) often have increased risk for perioperative complications such as infection or delayed wound healing. Because of this, the hospital team developed a comprehensive, high-risk, neuromuscular spine pathway to optimize patients prior to surgery in order to minimize risk and maximize their recovery.

Isaac pictured here with his parents Julie and Jason.
“Typically, a team of experts including orthopedic spine surgeons, plastic surgeons, neurosurgeons, intensivists, hospitalists, anesthesiologists, gastroenterologists, nutritionists, neurologists and pulmonologists collaborate to optimize a patient’s results,” said Dr. Ritzman. “In Isaac’s case, a feeding tube was placed to ensure he was nutritionally optimized to heal his surgical incision given that he had complex scarring over his spine from his surgical closure as an infant.”
Although Isaac frequently uses a wheelchair, he has a full body brace and is able to use a walker.
“He’s able to sit and push himself up the stairs with his upper body and can do his own transfers from his wheelchair,” said Julie.
While his feeding tube has stayed in place and is used for medication administration, Isaac enjoys all his favorite foods by mouth like mac and cheese, noodles and garlic bread. Now 13 years old and a newly minted 7th grader at Springfield Jr. High, Isaac is looking forward to learning more about his favorite subject – American history.
“Isaac is obsessed with George Washington,” said Julie. “We visited Mount Vernon, his home in VA and Isaac couldn’t get enough. He is constantly reading books and watching videos about all things related to American history.”
COVID postponed the Laupers plans to visit the Smithsonian’s natural history and American history museums, but Isaac spent some time fishing and camping this summer in his grandparents’ fifth wheel camper.

Isaac, who is an American history buff, enjoyed visiting Mount Vernon, the home of George Washington.
Julie says she’s grateful for the care Akron Children’s has provided.
“Isaac is doing well,” she said. “His digestion and posture are so much better. He has a better quality of life. Overall, he’s a pretty happy kid.”
For more information on the Spine Program and the innovative technologies being used to advance care for children and adolescents with abnormal curvature of the spine, visit akronchildrens.org.










