
Patrick celebrated his 9th birthday on August 18, 3 months after surgery that helped stabilize a painful curvature in his spine.
Patrick Carr is no stranger to doctors or to Akron Children’s for that matter. Born with neurofibromatosis, a genetic disorder that causes him to develop benign tumors in various areas of his body, he sees specialists in neurology, endocrinology and cardiology, and recently he added orthopedics to the mix.
It was in 2018 at an appointment with his endocrinologist, Dr. Kimberly Martin, that Patrick was referred to Dr. William Schrader, orthopedic surgeon, for evaluation because she noticed a curvature in his back.
“Patrick never complained about his back hurting and there was no curve that was visibly noticeable,” said Lori, Patrick’s mom. “We were pretty surprised to learn he had scoliosis.”

Patrick received his First Communion in August at St. Matthew’s Church in Ellet.
When the Carrs first met with Dr. Schrader, X-rays showed Patrick’s curve at 20 degrees. They were told to come back in 6 months so his curve could be rechecked to make sure it wasn’t rapidly progressing.
“When we went back his curve was worse and we were prescribed a Providence brace that Patrick had to wear every night,” said Lori. “He was only 6-years-old at the time and it was a real struggle. He hated wearing it and fought us every step of the way.”
Future follow-up appointments held more of the same news.
“His curve kept progressively getting worse,” said Lori. “He eventually ended up in a Boston brace which he had to wear 23 hours a day.”
Lori says Patrick’s neurofibromatosis likely contributed to the speed and severity of his worsening curvature. By spring 2019, he was referred to Dr. Todd Ritzman, an orthopedic surgeon who specializes in a type of surgery that uses magnetic rods for kids who are not done growing. Unlike teens who can have scoliosis fusion surgery, younger children need to have growth-friendly surgery to allow correction of the deformity while enabling the spine and thorax to continue to grow.
According to Dr. Ritzman, magnetic rod surgery is recommended for kids under age 10 when their scoliosis is severe or worsening despite a non-operative cast, brace, or physical therapy treatments.

Patrick, pictured here the day after his scoliosis surgery, was up and walking later that day. His mom says he recovered so well you wouldn’t know he just had surgery!
“Progressive early onset scoliosis is a challenging disorder because spinal fusion, our typical treatment for large curves, leads to immediate cessation in spine, chest and lung growth,” he said. “Consequently, we are not able to definitively fuse young children’s spines or we risk permanent lung and respiratory compromise.
“In Patrick case, magnetic growing rods were implanted through two minimally invasive incisions at the top and bottom of his spine to provide immediate correction of his deformity,” he added. “Following surgery, we are able to lengthen the rods in the outpatient setting at regular intervals.”
With the added complication of COVID and most elective surgeries postponed, Dr. Ritzman had to get special permission to operate on Patrick in May 2020.
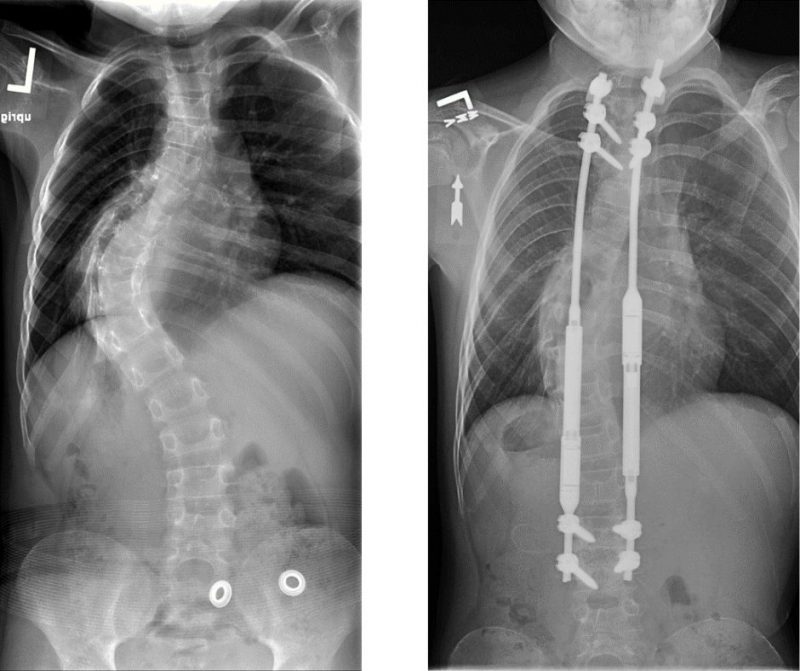
Patrick’s spine on the left, prior to surgery, and on the right, following the insertion of magnetic growth rods.
“Given the speed of Patrick’s curve progression, we chose to proceed with his surgery during the pandemic’s restricted phase to enable satisfactory, safe correction of his deformity and to avoid continued progression of his curve,” he said.
On May 21, Patrick underwent surgery and went home two days later.
“I was the only one allowed with him due to COVID,” said Lori. “I was amazed how quickly the nurses and therapists had him sitting in a chair and then up and moving around. He was moving so well you wouldn’t necessarily know he just had surgery.”
Patrick’s first post-operative appointment was virtual—a first for Dr. Ritzman.
“One of the unexpected benefits of the COVID pandemic has been the rapid advancements in virtual telehealth capabilities,” he said. “We are able to perform wound checks, examine walking and strength, and confirm patients are recovering well while avoiding the discomfort and inconvenience of car travel during the early postoperative course.

Patrick and his sisters Alexis, age 15, and Ashley, age 9, pose for a Christmas portrait in 2020.
“This is now standard practice,” he added. “Patrick helped us revolutionize our care!”
Patrick does need to go into the office for rod lengthening, which he has had twice so far—once in October and again in December. Depending on his growth, he may need the rods lengthened every 3 months.
“I was surprised how easy and painless it was,” said Lori. “Dr. Ritzman used an external magnetic remote control to rotate the screws which lengthen the rods. Since surgery, he has had his rods lengthened a total of 8 mm.”
By using magnetic growing rods instead of traditional growing rods, the goal is to eliminate the need for additional surgeries to lengthen the rods. Lori says she hopes Patrick’s rods will last until he is at least 13 when he will be a candidate for a permanent spinal fusion.
In July, 2 months after surgery, Patrick was fitted for a new brace at Hanger Clinic Prosthetics and Orthotics.
Last summer Patrick enjoyed being able to swim in the pool in his backyard and finally returning to school in-person in the fall.
“He has to be careful and isn’t allowed to jump, wrestle or rough house,” said Lori. “We don’t want him doing anything that could jar the rods out of place.”
Lori says the best part is no longer seeing her child in pain.
“Dr. Ritzman is extremely knowledgeable and Patrick loves him,” she said. “It’s great to have a doctor who not only is passionate about what he does but is passionate about his patients as well.”
Explore the treatments offered at the Spine Center , an Akron Children’s Center of Excellence.










