
In this file photo, Dr. Ananth Murthy examines patient Elijah Bell, as his mother, Colleen Bell, looks on. Eli underwent traditional ear construction in 2013-2015, which required rib cartilage as a donor and 3 separate stages. Now, our team is researching ways to utilize the remnant microtia cartilage along with a 3D printed biopolymer ear-scaffold. This will make the process of harvesting rib cartilage, as well as a multiple stage surgery unnecessary.
Hear this: Of the roughly 4 million babies born in the United States each year, an estimated 15% of them have an ear abnormality affecting the structure and appearance of part of or the entire ear, according to the American Academy of Pediatrics. Microtia, the most severe ear abnormality, occurs when the entire external ear is significantly smaller than usual or missing altogether.
In rare cases, children with microtia may experience frequent ear infections, a partial hearing loss and developmental delays. But for all of these kids suffering from the congenital birth defect, a critical concern is the negative impact on their self-esteem and social confidence with peers.
“Treating microtia is essential for the psychosocial development of a child,” said Dr. Ananth Murthy, director of pediatric plastic and reconstructive surgery and medical director for the Craniofacial Center and Speech Resonance Clinic at Akron Children’s. “Reconstruction of the external ear prior to school age can, in large part, prevent the negative psychological effects from peers, which has been shown to lead to social withdrawal, academic and behavioral issues.”
The problem is the risks for creating a new ear for these kids come with invasive procedures, tissue rejection and lifelong maintenance. So how can surgeons spare a child with an ear abnormality the risks and hurdles involved in the process of creating a new ear?
Dr. Murthy and his research team believe the sound solution is to grow a new one — one that will look and behave just like a normal ear — made from the child’s own tissue.
It’s a science called tissue engineering, and Dr. Murthy is spearheading this groundbreaking study with Akron Children’s staff scientist Qing Yu, PhD, in our Rebecca D. Considine Research Institute. He believes this is the future of regenerative medicine.
“Our goal is to develop a human ear with human tissue,” he said. “This breakthrough study would completely change the paradigm of ear reconstruction.”

Akron Children’s Staff Scientist Dr. Qing Yu with Pediatric Plastic and Reconstructive Surgeon Dr. Ananth Murthy
Problems with current ear reconstruction
For the last 50 years, the gold standard has been to recreate the ear framework using a patient’s own rib cartilage. It’s cumbersome and technically demanding because surgeons must physically carve it out to make it look like a real ear or recreate the missing portion of the ear.
The procedure uses the patient’s own tissue, so there’s significantly less risk the body will reject it. But, there are several downsides.
Complications can arise when removing the cartilage, and surgeons taking away valuable tissue from the ribs can cause donor morbidity, in rare cases. Not to mention, the procedure is invasive and time consuming because it must be done in stages and multiple surgeries.
What’s worse, after all that time and effort results are variable.
In recent years, a newer option to recreate the ear has become available. It involves a 3D printed ear using a porous polymer called polyethylene that allows the patient’s tissue to grow through it.
This newer option addresses many of the older procedure’s problems: it’s not done in stages, there’s no rib cartilage surgery and reduces the variability of the results. Sounds promising, right? Wrong.
“The biggest problem is it’s a foreign object, so the patient’s body is more likely to reject it. It also will require lifelong maintenance,” said Dr. Murthy. “We have 2 choices right now and neither of them are particularly great because they come with significant risks. So, we knew we needed to develop something better.”
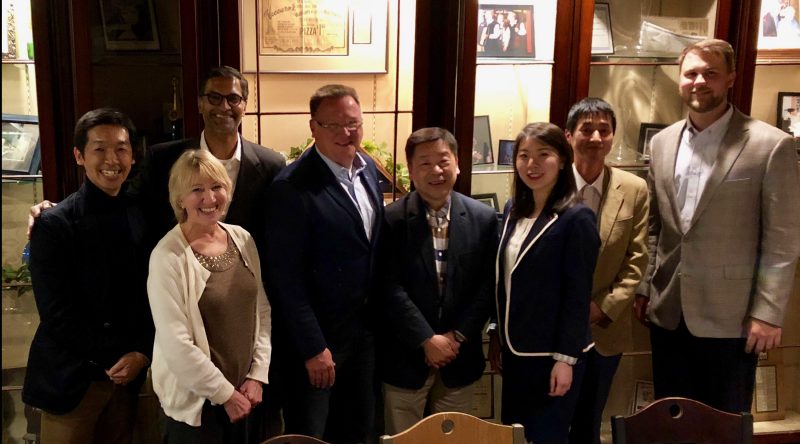
Dr. Murthy (third from left) and Dr. Qing Yu (third from right) stand with their Akron Children’s international ear reconstruction research team.
Forging the new frontier of tissue engineering
The research to regenerate a tissue-engineered ear was originally the brainchild of Dr. William Landis, PhD, a professor at Northeast Ohio Medical University (NEOMED) and The University of Akron. It involves first combining the patient’s own ear cartilage cells with a 3D printed, biodegradable, ear-shaped scaffold. The scaffold provides the structure for the cells to grow through. From there, surgeons in the operating room can then implant this engineered ear scaffold to complete the ear reconstruction.
Once the patient’s cells or tissues take over and the scaffold starts to degrade, the tissue will look and behave just like a normal ear. Because it’s made up entirely of the patient’s own tissue, after everything holds up during those 2 years it takes to degrade, Dr. Murthy and his team are confident the ear will last a lifetime.
“Similar to what you think of with building scaffolding, it’s a framework we can use to grow ear tissue using the patient’s own donated tissue, which is optimal,” said Dr. Murthy. “We don’t have something permanent that can cause rejection or infection, like the current polyethylene scaffold can. Another great benefit is the bio-polymer ear scaffold is especially strong; and unlike the polyethylene, it’s bendable and behaves like a typical external ear.”
Drs. Murthy and Yu are working closely with Northeast Ohio Medical University, partners in the U.S. and collaborators in Germany and Japan to bring this idea to life.
They are partnering with Gunze Limited in Japan, which manufactures particular polymers for cartilage engineering, as well as KLS Martin in Jacksonville and Germany. KLS is processing and supplying the scaffold that can be placed on a person. KLS tweaks the scaffold based on the team’s findings.
“Our goal is to come up with a safe and effective product that can help children with ear deformities,” said Dr. Murthy. “The team is feeling very encouraged, inspired and on the right track, but this kind of research takes time — 1% inspiration and 99% perspiration.”

Dr. Qing Yu works in the research lab on the breakthrough tissue engineering study.
Currently in animal trials, Dr. Murthy and his team are refining the scaffolds that would support cartilage growth.
Within the next couple of years, Dr. Yu hopes to find the right design for the scaffold so the study can be moved into clinical trials on patients, where they will use tissue donated by participating patients to generate cells through cell expansion to grow on the scaffold.
After performing many tests and experiments, the results are very promising.
“We have to make sure every single step makes sense and that it’s safe and effective,” said Dr. Yu. “Everything has to be well documented and deliberate. It’s painstaking, but rewarding.”
Rewarding indeed. This research could not only be groundbreaking for patients with Microtia, but for similar cartilage anomalies in every part of the body.
“There are so many different potential applications. You could use it for reconstructing a nose, ears, other parts of the face,and so on,” said Dr. Murthy. “Imagine being able to generate bone on a scaffold to replace bone that’s been destroyed by cancer, or a hip, or cartilage for a knee, or even create blood vessels. I really do believe this is the future.”
About the Rebecca D. Considine Research Institute
The Rebecca D. Considine Research Institute is the catalyst for pediatric research and innovation at Akron Children’s, northeast Ohio’s largest pediatric healthcare provider. With hundreds of clinical studies being conducted by investigators in more than 50 departments and specialties, research is part of the fabric of our culture. Our sole focus is on advancing the care for every child now, and for generations to come. Learn more at akronchildrens.org/research or follow the Research Institute on Twitter @ACHResearch.











